An integrated model with classification criteria to predict small-for-gestational-age fetuses at risk of adverse perinatal outcome
Abstract
Objective
To develop an integrated model with the best performing criteria for predicting adverse outcome in small-for-gestational-age (SGA) pregnancies.
Methods
A cohort of 509 pregnancies with a suspected SGA fetus, eligible for trial of labor, was recruited prospectively and data on perinatal outcome were recorded. A predictive model for emergency Cesarean delivery because of non-reassuring fetal status or neonatal acidosis was constructed using a decision tree analysis algorithm, with predictors: maternal age, body mass index, smoking, nulliparity, gestational age at delivery, onset of labor (induced vs spontaneous), estimated fetal weight (EFW), umbilical artery pulsatility index (PI), mean uterine artery (UtA) PI, fetal middle cerebral artery PI and cerebroplacental ratio (CPR).
Results
An adverse outcome occurred in 134 (26.3%) cases. The best performing predictors for defining a high risk for adverse outcome in SGA fetuses was the presence of a CPR < 10th centile, a mean UtA-PI > 95th centile or an EFW < 3rd centile. The algorithm showed a sensitivity, specificity and positive and negative predictive values for adverse outcome of 82.8% (95% CI, 75.1–88.6%), 47.7% (95% CI, 42.6–52.9%), 36.2% (95% CI, 30.8–41.8%) and 88.6% (95% CI, 83.2–92.5%), respectively. Positive and negative likelihood ratios were 1.58 and 0.36.
Conclusions
Our model could be used as a diagnostic tool for discriminating SGA pregnancies at risk of adverse perinatal outcome. Copyright © 2014 ISUOG. Published by John Wiley & Sons Ltd.
INTRODUCTION
Over the last decade, two different phenotypes of fetal growth restriction (FGR), determined primarily by the gestational age at onset of the disease and the pattern of umbilical artery (UA) Doppler indices, have been characterized1-4. In late-onset FGR, cardiovascular abnormalities do not extend beyond the cerebral circulation and normal, or only minimally elevated, UA Doppler indices are usually observed1, 2, 4, 5.
The distinction between milder cases of late-onset FGR from constitutionally small, but otherwise low-risk, fetuses is a clinical necessity. Since the identification of fetuses with late-onset FGR at an increased risk for adverse perinatal outcome cannot be based on UA Doppler indices, the use of other markers has been proposed. The use of middle cerebral artery (MCA) Doppler indices in this setting is supported by recent studies, which have demonstrated that 15–20% of term small-for-gestational-age (SGA) fetuses with normal UA Doppler have reduced impedance in MCA blood flow, and that this sign is associated with a poorer perinatal outcome6-8 and neurobehavior, both at birth and at 2 years of age9, 10. Furthermore, the cerebroplacental ratio (CPR), which combines the pulsatility indices (PI) of the MCA and UA, has been shown to be more sensitive to hypoxia than are its individual components, and it correlates better with adverse outcomes11-13. In addition to these Doppler parameters, abnormal uterine artery (UtA) Doppler has been associated with an increased risk of intrapartum fetal distress, emergency Cesarean delivery and admission to the intensive care unit7, 14, 15. Finally, evidence also exists that a very low estimated-fetal-weight (EFW) centile by itself predicts a higher risk of adverse perinatal outcome in term SGA fetuses without Doppler signs of brain redistribution and normal UA and UtA Doppler indices16, 17. A gap in current knowledge is the lack of information about the combined value of these parameters when used in an integrated model.
The objective of this study was to assess the value of combined obstetric, maternal and fetal features and Doppler parameters to define a set of criteria that can predict sonographically pregnancies with SGA fetuses that are at high risk for adverse outcome.
SUBJECTS AND METHODS
Between January 2008 and November 2012, consecutive patients with pregnancies suspected of having an SGA fetus were examined and recorded prospectively at the routine third-trimester scan, performed at the University Hospital Clinic, Barcelona, Spain. All pregnancies were dated according to first-trimester crown–rump length18. Inclusion criteria for this study were: (1) singleton pregnancy; (2) normal fetal anatomy; and (3) an EFW < 10th percentile according to local reference values19 at diagnosis of SGA after 32.0 weeks of gestation. Exclusion criteria were: (1) congenital malformations, including chromosomopathies and infections; (2) maternal consumption of illicit substances; and (3) contraindications for a vaginal delivery before the onset of labor (including the presence at inclusion, or development during follow-up, of absent or reversed UA diastolic flow). Controls (n = 513) were defined as singleton appropriate-for-gestational-age (AGA) pregnancies (EFW ≥ 10th centile according to local standards) at routine third-trimester ultrasound examination, and were sampled from our general pregnant population during the same period and matched 1:1 with cases by date of delivery (± 7 days). No Doppler evaluation was performed on controls. The study was approved by the local ethics committee and all women gave their informed consent to participate (IRB/2008/7315). The study design, analysis and reporting adhered to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) recommendations20.
In all study cases, fetal biometry and prenatal Doppler ultrasound examinations were performed by experienced operators using either a Siemens Sonoline Antares (Siemens Medical Systems, Malvern, PA, USA) or a Voluson E8 (GE Medical Systems, Zipf, Austria) ultrasound machine, equipped with a 6–2-MHz linear curved-array transducer. The EFW was calculated from the biparietal diameter, head and abdominal circumference, and femur length using the Hadlock formula21. The UA-PI was calculated from a free-floating portion of the umbilical cord. To minimize variability, the MCA-PI was measured in a transverse view of the fetal head, at the level of its origin from the circle of Willis22, and CPR was calculated as the ratio MCA-PI/UA-PI23. For UtA assessment, the ultrasound probe was placed on the lower quadrant of the abdomen, angled medially, and color Doppler imaging was used to identify the UtA at the apparent crossover with the external iliac artery. Measurements were taken approximately 1 cm distal to the crossover point. Doppler recordings were performed in the absence of fetal movements and voluntary suspended maternal breathing. All pulsed Doppler parameters were recorded automatically from at least three consecutive waveforms, with the angle of insonation as close to 0° as possible, and always below 30°. A high-pass wall filter of 70 Hz was used to record low flow velocities and to avoid artifacts. The last Doppler evaluation, within 1 week of delivery, was considered for analysis.
Follow-up was performed every 2 weeks in cases of normal CPR (≥ 5th centile23), weekly in cases of abnormal CPR and twice a week in cases of abnormal MCA (< 5th centile24). Induction of labor was recommended at 37 weeks' gestation for cases with abnormal CPR or MCA, otherwise at 40 weeks. Betamethasone was administered for pulmonary maturation in all cases delivering before 34.6 weeks. Cases with pre-eclampsia were delivered at 37 weeks or at diagnosis if identified after that gestational age.
Labor was induced by promoting cervical ripening with the administration of a slow-release prostaglandin E2 vaginal pessary (10 mg). If the onset of labor did not occur within 12 h, oxytocin induction was initiated. All deliveries were attended by a staff obstetrician blinded to the results of the Doppler parameters evaluated in this study. Indication for Cesarean delivery for non-reassuring fetal status was based on abnormal fetal heart-rate monitoring and abnormal fetal-scalp blood pH during intrapartum monitoring. Continuous fetal-heart monitoring was carried out and tracings were classified according to the following three-tiered system25: (1) normal: baseline of 110–160 beats per minute (bpm), variability > 5 bpm and absence of decelerations; (2) suspicious, i.e. the presence of one non-reassuring criterion out of: baseline, 100–109 or 161–180 bpm, variability < 5 bpm for less than 90 min, recurrent ( > 50% of contractions) typical variable decelerations for more than 90 min and a single prolonged deceleration for up to 3 min; or (3) pathological: more than one non-reassuring criterion or the presence of any abnormal feature, including: baseline of < 100 or > 180 bpm or sinusoidal patterns (for more than 10 min), variability < 5 bpm for more than 90 min, recurrent atypical variable decelerations for more than 30 min, late decelerations for more than 30 min and a single prolonged deceleration for more than 3 min.
In cases with a pathological fetal heart rate or a suspicious pattern not presenting a fetal heart-rate acceleration after digital fetal-scalp stimulation26, fetal-scalp blood sampling was performed and considered abnormal with pH values of < 7.15 or < 7.20 on two occasions 30 min apart. If cervical conditions did not allow fetal-scalp sampling, indication for Cesarean delivery was considered if an abnormal feature persisted after pessary withdrawal, oxytocin suspension and 10 min of intravenous infusion of ritodrine (200 µg/min). All cases with an adverse outcome were formally assessed to ensure that the management protocol had been followed correctly. Metabolic acidosis was defined as the presence of a UA pH < 5th centile (7.15) and a base excess greater than −12 mEq/L in the newborn27.
Statistical analysis
A predictive model for emergency Cesarean delivery because of non-reassuring fetal status or neonatal acidosis was constructed using the Decision Tree Analysis algorithm (SPSS 19.0, IBM, Armonk, NY, USA), which provides clinically comprehensive classification algorithms that allow their use in clinical practice to profile the individual risk for a given patient. The decision tree was developed using Exhaustive Chi-squared Automatic Interaction Detector (CHAID)28, a recursive partitioning method that builds classification trees for predicting categorical predictor variables by automatically selecting a cut-off for all the parameters, including: maternal age (years); body mass index (kg/m2); smoking (non-smoker vs smoker); nulliparity (no previous births < 22 weeks' gestation); gestational age at delivery (weeks); onset of labor (spontaneous vs induction); EFW centile29; UA-PI centile24; mean UtA-PI centile30; MCA-PI centile24; and CPR centile23. The classification and regression tree was constructed by splitting subsets of the dataset using all predictor variables, to create two child nodes, repeatedly. The best predictor was chosen using a variety of impurity and diversity measures. For a parsimonious model, the number of cases required to be present for a split has to be greater than 15% of the sample. A Bonferroni-adjusted chi-square test giving a P of ≤ 0.05 was used as the indicator of significance. The model was cross-validated by repeating the analysis over 10 random subsamples (leaving out one subsample each time) and constructing the tree from the average accuracy for cross-validated predicted classifications.
RESULTS
A total of 656 women fulfilled the inclusion criteria. Among them, 26 were excluded for breech presentation, 13 for having had more than one previous Cesarean delivery, 103 for absent/reversed end-diastolic velocity in the UA, and five for the presence of a medical contraindication precluding trial of labor, leaving a final population of 509 fetuses. Table 1 summarizes the demographic and perinatal characteristics of the included population of SGA pregnancies.
| Characteristic | Overall population (n = 509) | Non-adverse outcome (n = 375) | Adverse outcome (n = 134) | P* |
|---|---|---|---|---|
| Nulliparous | 321 (63.1) | 223 (59.5) | 98 (73.1) | 0.005 |
| Non-Caucasian ethnicity | 124 (24.4) | 96 (25.6) | 28 (20.9) | 0.29 |
| Maternal age at delivery (years) | 33.9 ± 6.1 | 33.7 ± 6.1 | 34.5 ± 6.1 | 0.22 |
| BMI at booking (kg/m2) | 22.3 ± 4.0 | 22.0 ± 3.7 | 23.1 ± 4.7 | 0.024 |
| Low socioeconomic level‡ | 120 (23.6) | 93 (24.8) | 27 (20.1) | 0.29 |
| Smoker at booking (≥ 1 cigarette/day) | 101 (19.8) | 80 (21.3) | 21 (15.7) | 0.17 |
| Alcohol consumption (> 170 g/week) | 7 (1.4) | 7 (1.9) | — | 0.20† |
- Data are given as mean ± SD or n (%). Paired comparisons:
- * t-test/Pearson-χ2 test or
- † Fisher's exact test.
- ‡ Routine occupation, long-term unemployment or never worked (UK National Statistics Socio-Economic Classification). BMI, body mass index.
Of these SGA pregnancies, there were 134 (26.3%) cases of adverse outcome, including, non-exclusively, 106 cases of emergency Cesarean delivery for non-reassuring fetal status (82 of which had abnormal fetal-scalp sampling) and 46 cases of neonatal acidosis. Table 2 shows Doppler parameters before birth and perinatal outcome according to the occurrence of adverse outcome.
| Parameter | Overall population (n = 509) | Non-adverse outcome (n = 375) | Adverse outcome (n = 134) | P* |
|---|---|---|---|---|
| UA-PI (Z-score) | 0.47 ± 1.4 | 0.44 ± 1.5 | 0.54 ± 0.9 | 0.669 |
| UtA-PI (Z-score) | 0.67 ± 1.7 | 0.46 ± 1.6 | 1.26 ± 1.7 | < 0.001 |
| MCA-PI (Z-score) | −0.10 ± 1.2 | 0.07 ± 1.2 | −0.58 ± 1.0 | < 0.001 |
| CPR (Z-score) | −0.91 ± 1.2 | −0.75 ± 1.2 | −1.34 ± 1.1 | < 0.001 |
| Induction of labor | 382 (75.0) | 269 (71.7) | 113 (84.3) | 0.004 |
| GA at delivery (weeks) | 38.4 ± 2.3 | 38.5 ± 2.4 | 38.1 ± 2.1 | 0.669 |
| Birth weight (g) | 2414 ± 441 | 2466 ± 429 | 2270 ± 443 | < 0.001 |
| Birth-weight centile | 4.5 ± 7.3 | 5.1 ± 7.7 | 2.7 ± 6.0 | < 0.001 |
| SGA confirmed at birth | 457 (89.8) | 329 (87.7) | 128 (95.5) | 0.011 |
| Pre-eclampsia | 59 (11.6) | 33 (8.8) | 26 (19.4) | 0.001 |
| Cesarean delivery | 146 (28.7) | 40 (10.7) | 106 (79.1) | < 0.001 |
| Operative vaginal delivery | 51 (10.0) | 32 (8.5) | 19 (14.2) | 0.063 |
| Cesarean delivery for NRFS | 106 (20.8) | — | 106 (79.1) | — |
| 5-min Apgar score < 7 | 6 (1.2) | 5 (1.3) | 1 (0.7) | 1† |
| UA pH at delivery | 7.23 ± 0.08 | 7.25 ± 0.05 | 7.17 ± 0.1 | < 0.001 |
| Neonatal acidosis | 46 (9.0) | — | 46 (34.3) | — |
| Admission to neonatal unit | 36 (7.1) | 21 (5.6) | 15 (11.2) | 0.03 |
- Data are given as mean ± SD or n (%). Paired comparisons:
- * t-test/Pearson-χ2 test or
- † Fisher's exact test. CPR, cerebroplacental ratio; GA, gestational age; MCA, middle cerebral artery; NRFS, non-reassuring fetal status; PI, pulsatility index; UA, umbilical artery; UtA, uterine artery.
The decision tree analysis (Figure 1) showed that cases with a CPR < 10th centile had the highest risk for adverse outcome (37.5% vs 19.1%; Bonferroni-adjusted χ2, P = 0.049). Among those with a normal CPR ( ≥ 10th centile), cases with a mean UtA-PI > 95th centile also had a significantly higher risk of adverse outcome (36.5% vs 15.6%; Bonferroni-adjusted χ2, P = 0.023). Finally, among the remaining group with a CPR ≥ 10th centile and a mean UtA-PI ≤ 95th centile, those with an estimated fetal weight < 3rd centile had a higher risk of adverse outcome (30.9% vs 11.4%; Bonferroni-adjusted χ2, P = 0.019).
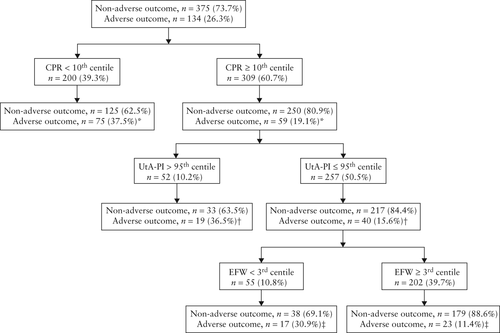
Cases were considered as low risk for an adverse outcome when they had a CPR ≥ 10th centile, a mean UtA-PI ≤ 95th centile and an EFW on at least the 3rd percentile. Cases were considered as high risk when any of these parameters was abnormal. The algorithm showed a sensitivity of 82.8% (95% CI, 75.1–88.6%), a specificity of 47.7% (95% CI, 42.6–52.9%), a positive predictive value of 36.2% (95% CI, 30.8–41.8%) and a negative predictive value for adverse outcome of 88.6% (95% CI, 83.2–92.5%). Positive and negative likelihood ratios were 1.58 and 0.36, respectively. Table 3 and Figure 2 display the Doppler parameters before birth and the perinatal outcome according to classification group for risk of adverse outcome, with the control group of AGA fetuses as reference.
| Parameter | AGA (n = 513) | Low-risk SGA (n = 202) | High-risk SGA (n = 307) | P* | P‡ |
|---|---|---|---|---|---|
| UA-PI (Z-score) | −0.13 ± 0.52 | 0.01 ± 0.54 | 0.77 ± 1.63 | 0.001 | < 0.001 |
| UtA-PI (Z-score) | −0.41 ± 1.3 | −0.17 ± 1.03 | 1.22 ± 1.80 | 0.019 | < 0.001 |
| MCA-PI (Z-score) | −0.16 ± 0.88 | 0.55 ± 0.99 | −0.53 ± 1.14 | < 0.001 | < 0.001 |
| CPR (Z-score) | −0.29 ± 1.2 | −0.17 ± 0.80 | −1.38 ± 1.11 | 0.19 | < 0.001 |
| GA at delivery (weeks) | 39.7 ± 1.3 | 39.2 ± 1.1 | 37.8 ± 2.7 | < 0.001 | < 0.001 |
| Birth weight (g) | 3447 ± 348 | 2683 ± 226 | 2236 ± 458 | < 0.001 | < 0.001 |
| Birth-weight centile | 57.6 ± 28.4 | 7.39 ± 8.35 | 2.56 ± 5.83 | < 0.001 | < 0.001 |
| Pre-eclampsia | 8 (1.6) | 7 (3.5) | 52 (16.9) | 0.109 | < 0.001 |
| Cesarean delivery | 78 (15.2) | 31 (15.3) | 115 (37.5) | 1 | < 0.001 |
| Operative vaginal delivery | 55 (10.7) | 16 (7.9) | 35 (11.4) | 0.26 | 0.2 |
| Cesarean delivery for NRFS | 25 (4.9) | 16 (7.9) | 90 (29.3) | 0.115 | < 0.001 |
| 5-min Apgar score < 7 | 3 (0.6) | 2 (1.0) | 4 (1.3) | 0.558† | 1† |
| UA pH at delivery | 7.23 ± 0.16 | 7.24 ± 0.06 | 7.22 ± 0.08 | 0.388 | 0.003 |
| Neonatal acidosis | 31 (6.0) | 10 (5.0) | 36 (11.7) | 0.572 | 0.009 |
| Admission to neonatal unit | 20 (3.9) | 8 (4.0) | 28 (9.1) | 0.969 | 0.026 |
- Data are given as mean ± SD or n (%). Paired comparisons: AGA vs low-risk SGA compared using
- * t-test/Pearson-χ2 test or
- † Fisher's exact test; low-risk SGA vs high-risk SGA compared using
- ‡ t-test/Pearson-χ2 test or Fisher's exact test. CPR, cerebroplacental ratio; GA, gestational age; MCA, middle cerebral artery; NRFS, non-reassuring fetal status; PI, pulsatility index; UA, umbilical artery; UtA, uterine artery.
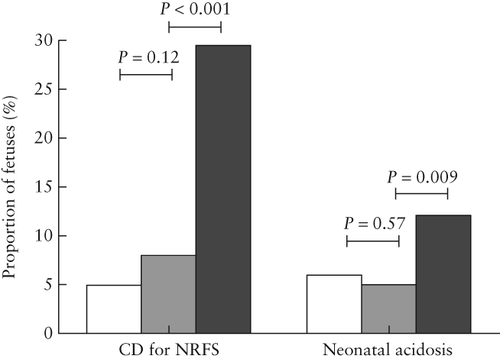
 ) and high-risk (
) and high-risk ( )) and appropriate-for-gestational-age (AGA,
)) and appropriate-for-gestational-age (AGA,  ) fetuses according to classification of risk for adverse outcome. Groups compared using Pearson-χ2 test. CD, Cesarean delivery; NRFS, non-reassuring fetal status.
) fetuses according to classification of risk for adverse outcome. Groups compared using Pearson-χ2 test. CD, Cesarean delivery; NRFS, non-reassuring fetal status.DISCUSSION
In this paper we propose criteria for defining high risk for adverse outcome in SGA fetuses, derived from analyzing a large cohort of SGA fetuses delivered near term. The impact of identifying at-risk growth-restricted fetuses from the general population of SGA fetuses cannot be underestimated, considering that SGA affects up to 10% of deliveries in developed countries and represents approximately 400 000 cases per year in Europe alone.
In our study, UA Doppler indices did not differ between SGA fetuses with or without adverse perinatal outcome. This adds to the body of evidence showing that this parameter does not reliably reflect placental insufficiency and does not predict adverse outcome in late-onset intrauterine growth restriction2, 31.
Recent research has demonstrated that up to 20% of term SGA fetuses with normal UA Doppler have abnormal MCA Doppler, probably secondary to fetal hypoxia8. While the degree of placental insufficiency leading to such hypoxia is not reflected in the UA, it exposes the fetus to an increased risk of adverse perinatal outcome7, 8, 15 and may have consequences on its neurodevelopment9, 10. These studies support the use of brain Doppler evaluation to distinguish late-onset FGR from constitutionally small fetuses. We have previously shown that induction of labor in SGA cases with isolated MCA Doppler abnormalities is associated with an increased risk of fetal distress and neonatal acidosis8. Thus, it was expected that CPR, as a more sensitive marker of hypoxia, would be the first parameter to enter our decision tree11, 12.
Second, in our model, UtA Doppler divided the population with a normal CPR into two groups of significantly different risk for adverse outcome. In a recently reported longitudinal series32, approximately one-third of abnormal third-trimester uterine Doppler studies occurred in women with normal scans during the second trimester, suggesting that a proportion of placental disease emerges late in pregnancy. Hence, the potential advantage of a third-trimester Doppler ultrasound scan is the ability to detect placental insufficiency of differing pathways. Our finding that abnormal Doppler indices in the UtA are associated with adverse perinatal outcome, is consistent with a previous report showing that abnormal velocimetry in the UtA and MCA are independently correlated with the occurrence of emergency Cesarean delivery7.
Third, severe growth restriction, as reflected by an EFW < 3rd centile, further improved the risk stratification in the subgroup in which CPR and UtA Doppler parameters were both normal, allowing us to optimize the diagnostic criteria. We have previously shown that in SGA fetuses with normal CPR and UtA Doppler, an estimated weight < 3rd centile confers a four-fold increased risk of fetal distress and acidosis when compared to SGA fetuses with a percentile above this cut-off value17.
The finding that SGA fetuses at high risk had a five-fold higher incidence of pre-eclampsia supports the concept that this category corresponds with latent placental insufficiency not reflected in the UA but that confers a lower tolerance to labor. This is in keeping with other series on late-onset SGA with data on placental histology33.
The clinical relevance of using a combined model over a single predictor is that it provides a significant improvement in prediction without excessive technical sophistication; estimation of fetal weight is an integral part of the third-trimester scan, and Doppler interrogation of the UA, MCA and UtA is easily accomplished in a great majority of cases. This algorithm allows for the profiling of the general population with late SGA in two groups at different risk: while SGA fetuses with moderate growth restriction ( ≥ 3rd centile) and normal placental function on both the fetal (normal CPR) and maternal (normal uterine Doppler) sides could be considered low risk and managed as constitutionally small babies, those with either severe growth restriction or evidence of placental dysfunction should be considered at higher risk. In our series, SGA fetuses at low risk accounted for 40% of the study population, in which only 17% of the adverse outcomes occurred, whereas SGA fetuses at high risk represented the remaining 60% of the study population, in which 83% of the instances of adverse outcome were found.
A large trial carried out in The Netherlands on late-SGA pregnancies, comparing systematic induction at term with expectant management, showed no differences in the perinatal and neonatal outcomes between the strategies34, 35. This evidence has been translated into guidelines as a general recommendation for the induction of labor at 37–38 weeks' gestation36-38, with the rationale of avoiding the rare, but devastating, instances of stillbirth. However, with such a strategy, a large fraction of constitutionally and healthy SGA babies are unnecessarily induced, which has the potential to result in lower satisfaction and poorer fulfilment with the birth experience39. Despite the low positive predictive value and likelihood ratio, our algorithm showed a good capacity to rule out perinatal adverse outcome, as reflected in the negative predictive value and likelihood ratio, which suggests that it would be suitable for risk stratification to select women for expectant management.
We acknowledge that there are some limitations to our study. It could be argued that the fact that, in most cases, labor was induced may affect the external validity of our results by increasing per se the risk of Cesarean delivery. However, results from a large trial on late SGA showed no differences whatsoever in the rate of Cesarean delivery when systematic induction beyond 36 weeks was performed, compared with expectant management35. Furthermore, we do not have information on the use of oxytocin for labor augmentation, which may also have played a role as a risk factor for fetal distress.
Another limitation is that Cesarean delivery for non-reassuring fetal status and, to a lesser degree, neonatal acidosis, is a soft proxy for adverse outcome. Other series have failed to find an association between term SGA and short-term neonatal hard outcomes, such as hypoxic-ischemic encephalopathy40. The study was underpowered to evaluate these outcomes. It could be argued that the occurrence of an abnormal cardiotocograph prompts an emergency Cesarean delivery that, in turn, prevents overt adverse outcome, so these are competitive risks. This limitation could be overcome by combining these two outcomes into a composite outcome. Furthermore, we believe that non-reassuring fetal status is a finding that has an impact on the delivery management of SGA babies. In addition, some studies have revealed an increased risk of maternal and neonatal consequences following an emergency Cesarean delivery41, 42. Moreover, despite our attempt to address confounding by entering a set of clinical variables (such as nulliparity or body mass index, which differ between cases with and without adverse outcome) in the multivariate analysis as candidate predictors, we acknowledge that it would have been a more robust design to have matched the groups by these potential confounders. Finally, the analysis automatically selected a non-conventional cut-off centile for CPR (the 10th instead of the 5th centile), which may limit the clinical applicability of our model. This could be overcome easily by using supporting software, such as that available at: http://medicinafetalbarcelona.org/en/research/resources.
In conclusion, the model developed here could be used in the risk stratification of pregnancies suspected prenatally of having late-onset SGA. The model is based on standard fetal biometrics and Doppler parameters that can be obtained readily in most clinical settings.
ACKNOWLEDGMENTS
The study was supported by grants from the Fondo de Investigación Sanitaria (PI/060347) (Spain), the Cerebra Foundation (Carmarthen, Wales, UK) and the Thrasher Research Fund (Salt Lake City, USA). This study was also partially supported by grants from ‘Fundació la Caixa’.