The role of the multidisciplinary team in surgical management of intractable tubo-ovarian abscess as a late sequelae of challenging Crohn's disease in the modern era: A case report and review of current literature
Abstract
Chronic, severe Crohn's disease in a young female patient can result in surgical complexity. The rarity of the presentation of intractable pelvic abscesses within this etiology with additional considerations given to fertility concerns and hence requirement for input from a multi-disciplinary team makes this a vital case in building a consensus for evidence-based surgical management. A 29-year-old nulliparous woman was referred to our tertiary centre for surgical management of Crohn's disease with known tubo-ovarian abscess and abdominoperineal and abdominal wall sinuses. Her previous surgical history included 4 midline laparotomies, subtotal colectomy and proctectomy with stoma formation. The patient underwent egg collection to preserve fertility. This was followed by midline laparotomy and abdominoperineal resection, which involved a retrograde radical modified hysterectomy using the Hudson technique, alongside excision of the perineal sinus, with reconstruction of the perineal defect using an internal pudendal artery perforator gluteal fold flap, and in addition to excision and drainage of the abdominal wall abscess. Involvement was sought from gynecological oncology, colorectal, urology, plastics, stoma, fertility, microbiology, and gastroenterology teams, which enabled successful preservation of end organ function and improvement in patient psychological well-being. This case is a paradigm of surgical challenge, requiring expert gynecological oncology techniques including a retroperitoneal approach, nerve and vessel sparing considerations alongside colorectal and urological procedures. Moreover, we believe that our blueprint for effective multi-disciplinary practice will inform the future management of gynecological surgery. Therefore this report aims to contribute towards the optimum management of the gynecological sequelae of Crohn's disease.
1 INTRODUCTION
Crohn's disease and its associated immunological sequelae can present a unique challenge in cases requiring surgical intervention. Surgery is a last resort, acknowledging not only an increase in the risk of a patient requiring further surgical management but also of complications from other prior interventions. Tubo-ovarian abscesses (TOAs) rarely present as a manifestation of Crohn's disease, with very few cases identified in the literature.1, 2 Moreover, the previous focus was on their unique presentations, without detailing required surgical input. The European Crohn's and Colitis Organization (ECCO) guidelines on therapeutics in Crohn's disease have identified that at least half of patients will undergo surgical management, with the best outcomes achieved by expert centers who can provide an individualized approach.3 As illustrated in our case, ECCO detail that immunosuppression may be hazardous, with antibiotics rarely being effective and drainage having a risk of failure. However, there remains outstanding the identification of a consensus approach to intra-abdominal abscesses.
We detail the stepwise management of a young female patient with complex Crohn's disease and our definitive treatment. We highlight the great dichotomy of surgical challenges faced in this age group, whilst acknowledging fertility concerns. Further details are provided on an approach to the battlefield abdomen in chronic inflammatory disease and the late consequences of delays in treatment. We also provide a summary of the available literature and areas for further consideration, with the aim of providing patient-centered, evidence-based care. This is a seminal case in identification and treatment of the grave consequences of rare sequelae of Crohn's disease. This complex presentation in conjunction with the background etiology and subsequent requirement for multidisciplinary collaboration highlights the need for a consensus for optimal management.
2 CASE PRESENTATION
We present the case of a 29-year-old nulliparous female who was referred for consideration of surgical management of a pelvic abscess in the right iliac fossa. For this case, ethical approval and patient consent have been sought. She has a previous medical history of Crohn's disease and renal impairment secondary to subsequent interventions, which was first diagnosed aged 12. Her previous surgical history includes an emergency midline laparotomy for stricture and obstruction in 2014, with right-sided colonic diversion and formation of stoma. At subsequent sigmoidoscopy, a bowel perforation occurred, which warranted a repeat emergency midline laparotomy, exploration and washout. Further flares of her Crohn's disease required yet a third midline laparotomy and colectomy with refashioning of stoma. A fourth laparotomy in 2019 was performed for proctectomy due to issues with a discharging perineal sinus and also included refashioning of the stoma to the left side and further resection of active Crohn's disease. Due to the extent of disease and multiple interventions the patient developed right-sided renal tract outflow obstruction for which she underwent a nephrostomy. This was subsequently treated with a right-sided anterograde ureteric stent. Her drug history includes folic acid, Rigevidon, prophylactic broad-spectrum antibiotics, omeprazole and Ensure sachets. She is a non-smoker, abstains from alcohol and has a body mass index (BMI, calculated as weight in kilograms divided by the square of height in meters) of 18.
Despite the extensive course of surgical treatment, the patient developed a symptomatic intractable pelvic abscess, due to the transmural inflammation and penetration of the bowel wall noted in Crohn's disease, which in turn led to a contained perforation. Unfortunately, attempts at radiological drainage of this abscess were unsuccessful, warranting referral to our tertiary center. On examination, the patient's abdomen was extensively scarred, with multiple laparotomies and a stoma on the left side (Figure 1). She had also developed a right-sided groin collection arising from the pelvic sidewall alongside a discharging sinus of the perineum following previous anal excision (Figure 2). Whilst an overt fistula was not identified, there was noted to be a 4 cm area of inflammation. A stoma scar was also present on the right lower abdomen and there was evidence of delayed wound healing. Bimanual examination revealed a large central pelvic mass, which most likely involved the uterus and ovaries and was inseparable from a suspected residual rectal stump.


The team undertook a panel of investigations including blood tests and an infection screen, all of which were negative, indicating a sterile inflammatory abscess process. A magnetic resonance imaging scan was also undertaken, which showed a tract containing fluid within the pelvis, extending from the small bowel to the perineal flap. Separate small pelvic fluid collections not amenable to percutaneous drainage were also noted.
Given the complexity of the case, a multidisciplinary team (MDT) meeting was arranged involving the gynecological oncology, colorectal, urology, plastic surgery, stoma and fertility teams. Input was also obtained from microbiology, gastroenterology and anesthetic teams to ensure both preoperative surgical and Crohn's status optimization. Whilst having historically been treated with immunosuppressant and biologic therapy (including infliximab and adalimumab to minimal effect), this had been ceased prior to surgery. It was agreed that, if the small bowel was unaffected by disease process, then the patient would not benefit from further medical treatment. Preoperatively, the patient underwent ultrasound-guided egg collection in consideration of fertility preservation.
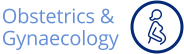
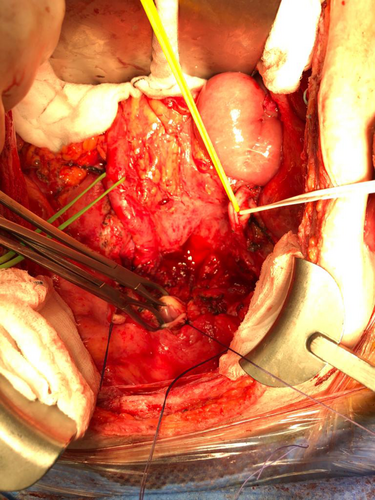
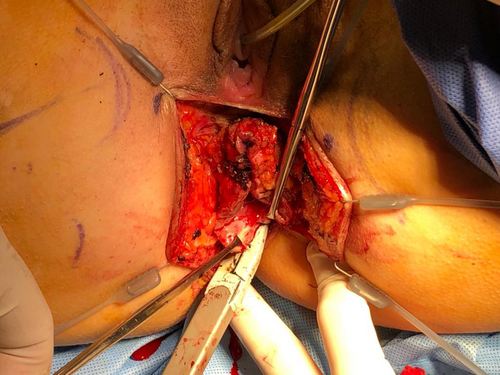
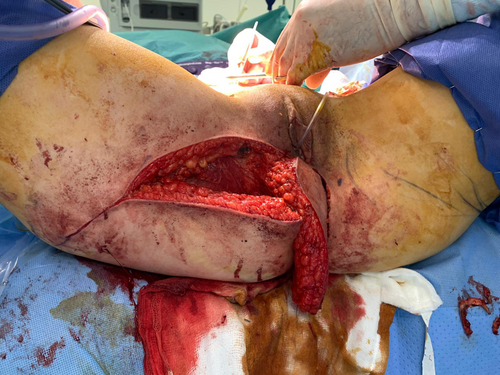
Under general anesthetic and in modified Lloyd Davis position, the patient underwent midline laparotomy. Significant adhesions were noted throughout the abdomen and pelvis with the left ovary and tube encased within the pelvic sidewall. A stented and hypertrophied right hydroureter was noted with a left duplex ureter (Figure 3). Despite use of cold scissor technique, an inadvertent enterotomy was noted and repaired. Access to the pelvis involved a retroperitoneal approach with bilateral ureterolysis and retrograde modified Hudson technique to complete the hysterectomy and bilateral salpingo-oophorectomy (Figure 4). Abscess process was noted to be connecting the uterus to the right ovary (Figures 5 and 6). The perineal sinus was excised (Figures 7 and 8) and the defect reconstructed using an internal pudendal artery perforator (IPAP) gluteal fold flap, ensuring that there was no ongoing communication with the peritoneal cavity (Figures 9 and 10). Additional surface abscesses were noted along the lower pole of the previous midline scar, alongside two in the right lower quadrant. These were opened and excised, with evidence of collection into the cavity from the pelvis via an inguinal ligament sinus. A ‘redivac’ drain was inserted via this sinus in addition to two gluteal drains and a Robinson's drain into the pelvic cavity.




Postoperatively, the patient was treated with broad-spectrum prophylactic antibiotics; however, we noted of interest that deep wound swab cultures reported no growth. All drains were removed upon achievement of minimal output. The patient received venous thromboembolism prophylaxis and hormonal replacement therapy. Due to loin pain and dysuria, despite negative investigations, the ureteric stent was replaced. The patient was discharged on day 10. She continues to have 6-monthly stent changes with prophylactic low-dose antibiotic cover for recurrent urinary tract infections (with no evidence of fistula on magnetic resonance enterography). The patient also reports a 5 mm minimally discharging (and spontaneously improving) sinus in the posterior junction of the natal cleft and flap, which is lined by chronic granulation tissue and presented 6 months postoperatively. The patient's abdominal wounds have otherwise healed well with no evidence of further collection, new lesions or local/regional recurrence.
3 DISCUSSION
This case highlights the grave consequences that are brought forth as a result of longstanding Crohn's disease. In this specific case, the associated immunological processes of the disease further aggravated the aforementioned late sequelae, particularly following multiple surgical interventions. These complications were managed by further procedures alongside years of antibiotics and immunosuppressants without success, and still further exacerbated by delays in treatment, as teams were hesitant to intervene on such a hostile abdomen. This highlights the paradigm of surgical challenge in Crohn's disease wherein the disease complicates the surgery and the surgery complicates the disease.4 This case highlights how a disease that is assumed to largely affect the gastric system can go on to cause dysfunction across the bio-psychosocial health of an individual. Finally, our successful management of this case identifies how definitive treatment is often necessary to improve a patient's quality of life and how a multidisciplinary approach is needed to provide such treatment.
The ECCO guidelines for medical treatment of Crohn's disease identify a stepwise approach to remission.5 Aminosalicylates are recommended for patients with mild to moderate Crohn's disease, especially in the presence of colonic involvement, as they act by reducing inflammation in the lining of the intestine. Corticosteroids are recommended for short-term use in patients with moderate to severe Crohn's disease who are not responding to aminosalicylates, reducing inflammation throughout the body. The next steps on the ladder include immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate, which suppress the immune system and, finally, biologics, which target specific proteins involved in inflammation and include medications such as infliximab, adalimumab, and vedolizumab. For maintenance in patients with mild disease there is no evidence to suggest an optimum treatment with conservative management advised, whereas in moderate to severe disease in remission, immunomodulators and biologics have been identified as most effective, with aminosalicylates and steroids lacking efficacy alongside an increased risk of adverse effects. It has been identified that treatment decisions should be made in consultation with the patient to ensure that treatment goals are aligned with patient preferences. In the case of our patient, it was decided that as previous immunotherapy had been ineffective, further therapeutics would not be considered.
The guidelines recommend that surgical treatment for Crohn's disease should be considered when medical therapies fail or complications arise, or in cases of fistulas, or abscesses.3 They provide recommendations for various surgical procedures, including stricturoplasty, resection, and stoma surgery. The choice of surgery should be based on the location and extent of disease, the presence of complications, and the patient's overall health status. Strictures that are short, non-penetrating, and non-inflammatory can be treated with stricturoplasty, a procedure that widens the narrowed segment of the intestine without removing it, thereby preserving bowel length and function. Resection involves removing the affected segment of the intestine and is used when there are complications such as abscesses or fistulas. In certain cases, a stoma may be created, which involves bringing the intestine through the abdominal wall to create an opening for waste elimination.
The management of a TOA typically involves a combination of antibiotics and drainage, either by needle aspiration or surgical intervention. Broad-spectrum antibiotics are usually prescribed to treat infection associated with TOA. In more severe cases, drainage of the abscess may be necessary to help alleviate symptoms and promote healing. This can be done either by needle aspiration under image guidance or by surgical intervention. Percutaneous drainage is advised as the primary treatment option for well-defined unilocular abscesses and has reported success rates of 74%–100%,6 often avoiding the need for subsequent emergency surgery. Often percutaneous drainage is advised as a bridge to elective surgery, as emergency surgery has a higher risk of complications. Current identification of those requiring further surgery relies on clinical judgment with recurrence being 6.5 times greater when surgical resection is not conducted.7 Factors associated with failed medical management include larger abscess size, increased age, parity, initial elevated white blood cell count and bilaterallity of abscesses.7, 8 A scoring system has been proposed by Yongue et al. (Table 1) to predict medical management failure, which incorporates temperature, C-reactive protein, and TOA diameter.8 In this study, including a total of 214 consecutive patients, a score of 4 or more was predictive of the need for surgical or radiological intervention, with a sensitivity of 69% and a specificity of 88%. In some cases, surgical intervention may be necessary to remove the abscess alongside associated tissue damage. This may involve a laparoscopic procedure or an open surgery, depending on the severity of the abscess and the patient's comorbidities. Following initial management, regular monitoring with imaging and examinations may be necessary to track the progress of the infection and to evaluate treatment efficacy.
| Points | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Temperature (°C) | <37 | 37 ≤ X ≤ 38 | 38 ≤ X ≤ 38.5 | ≥38.5 |
| Tubo-ovarian abscess size (cm) | <5.5 | 5.5 ≤ X ≤ 8.5 | 8.5 ≤ X ≤ 10.5 | ≥10.5 |
| C-reactive protein (mg/L) | <250 | — | ≥250 | — |
Perineal complications are relatively common in patients with Crohn's disease and include fistulas, abscesses, fissures and strictures. Perineal Crohn's disease is associated with a poorer prognosis and higher rates of disease recurrence, hospitalization, and surgical intervention.9 Medical management including antibiotics, immunosuppressive drugs, and biologic therapies may be used to reduce inflammation and promote healing in the affected area. Therapeutic adjuncts include lifestyle changes, pelvic floor physical therapy and psychological support to cope with the emotional impact. The ECCO guidelines recommend that surgery should be considered for patients with perianal Crohn's disease who have had failed medical therapy or have severe, complicated disease.3 Surgical options include fistulotomy, seton placement, rectal advancement flap, and proctectomy. Fistulotomy involves incising the fistula tract and draining the abscess in cases of simple or superficial fistulas. Seton placement involves placing a rubber or synthetic tube through the fistula tract to maintain and allow for drainage, for complex or recurrent fistulas. The rectal advancement flap procedure involves the use of healthy tissue from the rectum to cover the fistula tract and promote healing and is best suited for complex, high-risk, or recurrent fistulas. Finally, proctectomy involves removing the rectum and anus in cases where the disease is severe or recurrent. In the case of our patient, an IPAP gluteal fold flap was utilized as it is excellent for reconstruction following extensive perineal defects. Its sufficient soft tissue volume allows restoration of cosmetic shape and function, ensuring a reliable blood supply to support healing and minimize donor-site morbidity.10, 11
Crohn's disease can also cause a significant degree of dysfunction to the urological system, with 1 in 10 patients with inflammatory bowel disease going on to develop chronic kidney disease within 10 years of diagnosis, alongside an increased risk of acute kidney injury and kidney stones.12 Urological complications of Crohn's disease can occur due to inflammation, scarring, and fistula formation. Common complications include ureteral obstruction, urinary tract infection, bladder inflammation, fistulation and kidney stones. Management options include regular monitoring alongside medical management in the form of antibiotics and immunosuppression as appropriate and surgical management if required. In this particular case, the unusual anatomy of a duplex ureter and complex adhesive processes exemplified the surgical challenges of this battlefield abdomen. However, surgery was vital in order to prevent further abscess pathology leading to ureteric obstruction.
The ECCO guidelines stress the importance of a multidisciplinary approach involving gastroenterologists, surgeons, and radiologists to ensure that patients receive appropriate and timely surgical care.3 In surgery, the MDT approach is of particular importance for ensuring optimal patient outcomes.13 Such benefits include increased efficiency, enhanced safety and more comprehensive postoperative care.14 A case series by Horvath et al. details how the MDT approach in gynecological oncology not only ensures that patients are seen by appropriate teams but also reduces time from initial referral to evaluation.15 However, they also identified challenges associated with multidisciplinary working, including difficult communications, increased resource requirement, resistance to change and difficulty engaging patients in this approach. Despite this, there are methods to overcome these barriers, including regular meetings to facilitate communication, additional staff and funding allocation, standardized protocols and education for both professionals and patients to support engagement.16 The complicated nature of this case required a tertiary center MDT and our center allowed a range of specialist teams to work in conjunction and undertake the procedure together. The gynecological oncology specialists gathered the wider team and focused on the excision of the TOA. The plastics team supported the excision of the perineal sinus and the creation of the reconstructive flap. Furthermore, the urological team were involved in ureterolysis and stent management, and the colorectal team assisted in adhesiolysis, stump excision, small bowel repair, and stoma refashioning. The gastroenterology team continue to support the patient in the management of her Crohn's disease. Additional teams were involved in pre- and postoperative care, including fertility preservation and stoma management, physiotherapy, and pain management.
During the management of this case, we have placed the patient at the center of her care. This was vital due to the dichotomy of need for invasive and potentially debilitating treatment in a young patient. Significant aspects of this included hormone replacement therapy and fertility preservation. Preoperative egg harvesting and extensive counseling were therefore of the upmost importance. According to a review by Tschudin et al., fertility preservation was considered to be a vital aspect of discussion around care to many young patients with life-threatening diseases, a concern mirrored by their healthcare professionals.17 However, many patients subsequently identified a knowledge deficit regarding fertility preservation, with some studies showing recall of fertility counseling as low as 34%.17 Important issues identified to discuss during counseling include pre-existing psychological stressors, choice of fertility preservation strategies in the face of uncertain future relationships, decision-making regarding the use of third party reproductive systems (egg donation and gestational surrogacy), treatment expectations regarding pregnancy or miscarriage, ethical issues pertaining to the handling of embryos, and decision regret by patients who decline fertility preservation.18 During these consultations, it has been identified that most patients have positive experiences during counseling; however negative experiences are often associated with reduced time for counseling, not having the opportunity to address all concerns, not feeling supported by the counselor, and not all applicable options being discussed.19 Therefore, decisions regarding fertility in young women are complex and require a patient-centered approach, with enough time for deliberation. This patient-centered approach also extended to her follow-up care when addressing further management of her disease, with consideration being given to her wish to avoid further surgical input for ureteric dysfunction and immunological medications.
4 CONCLUSION
In conclusion, we present a unique case of TOA secondary to longstanding Crohn's disease. We propose an effective surgical strategy for managing this condition with a focus on support from members of the MDT. This case also highlights the grave sequelae of delayed Crohn's disease management and complications that can arise secondary to this. Therefore, a patient-centered focus is needed in their management to ensure the best possible outcomes. Due to the rare nature of this complication, we have also identified that further research is needed into the management of this condition; specifically, regarding evidence-based assessments of optimum surgical input and maintenance of remission thereafter.
AUTHOR CONTRIBUTIONS
Shanghavie Loganathan: literature review, manuscript, submission; Sarah Louise Smyth: figures, manuscript, review; Roman Mykula: review; Hooman Soleymani: figures, review. Soleymani Majd: conceptualisation, manuscript, leading surgeon, supervision.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.